Access to funding and other resources can make or break technology implementations. Rising costs, low margins, shifting reimbursements, budget constraints and other daunting financial barriers stand between healthcare organizations and the digital transformations they dream of executing to improve patient care—but these obstacles can be overcome.
Research conducted by HIMSS Market Insights revealed the disparities between the largest hospital systems, with billion-dollar revenues and thousands of beds, compared to smaller care settings with less than $500 million in revenue and fewer than 500 beds. The survey, “Targeting the Biggest Bang for the Buck,” looked across the healthcare spectrum to measure leaders’ financial outlooks as they pursue technological investments to advance their strategic priorities over the next year.
In this blog, the second of a three-part series, we’ll explore how healthcare’s haves and have-nots approach digital transformation differently according to the HIMSS survey, which spanned executives, IT/tech directors, clinical leaders and clinicians at hospitals, clinics, academic medical centers and healthcare systems of all sizes.
Assessing the size advantage
Across the board, only a quarter of healthcare organizations (26%) are confident in their financial readiness to tackle their strategic objectives over the next 12 months. But their available resources play a big role in their confidence.
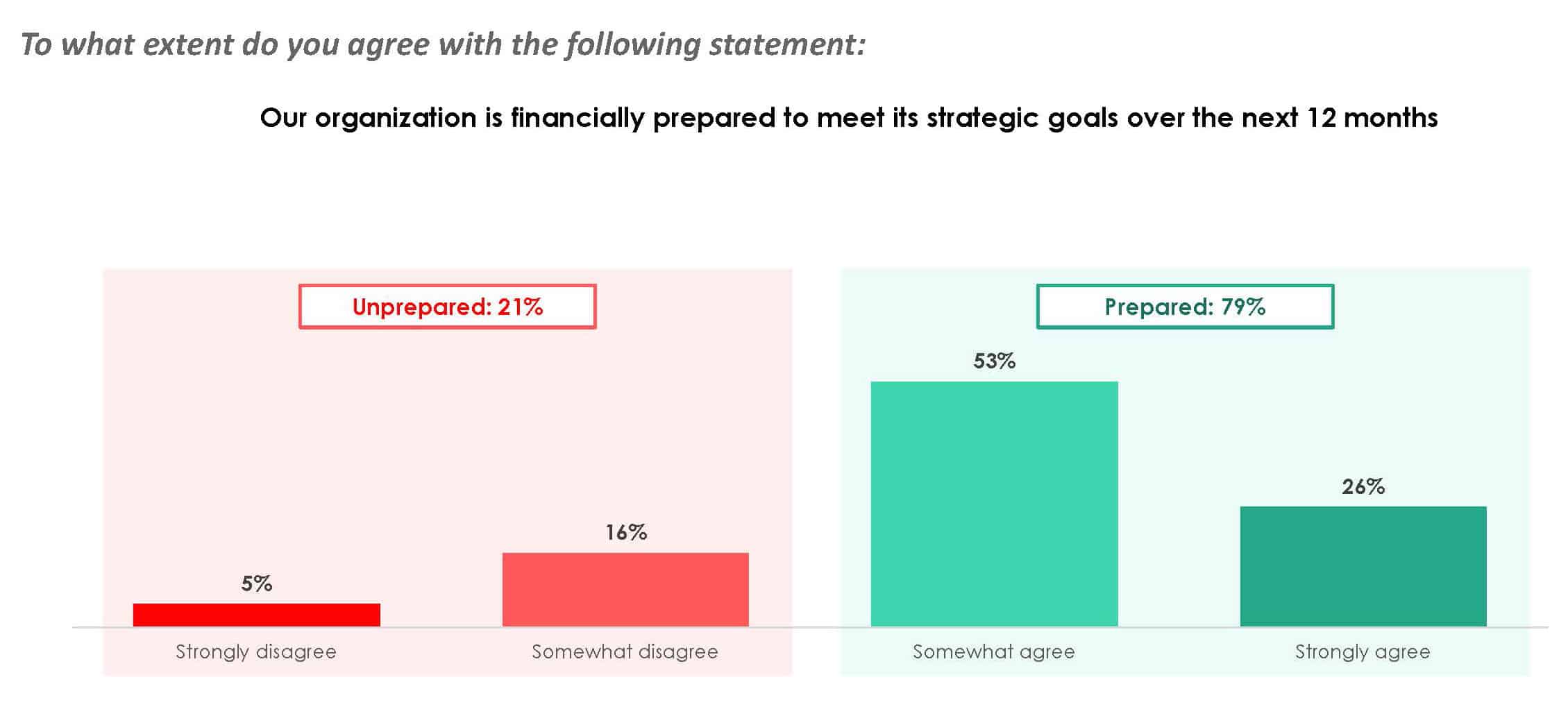
Not surprisingly, the survey showed that larger organizations are more likely to feel financially prepared to meet their strategic initiatives than smaller ones. Specifically, about nine out of 10 healthcare organizations with more than $501 million in revenue feel financially prepared, compared to only 67% of organizations with revenue of $500 million or less. Similarly, about nine out of 10 organizations with more than 1,000 beds report strong financial footing, compared to 72% of organizations with fewer than 1,000 beds.
Larger organizations undoubtedly benefit from greater budgets, bigger IT teams and specialized expertise for implementing advanced technology solutions. They also employ economies of scale, allowing them to negotiate better pricing and spread the cost of implementation across a larger patient base. Plus, they often use more sophisticated systems to make data-driven decisions and measure the impact of their investments.
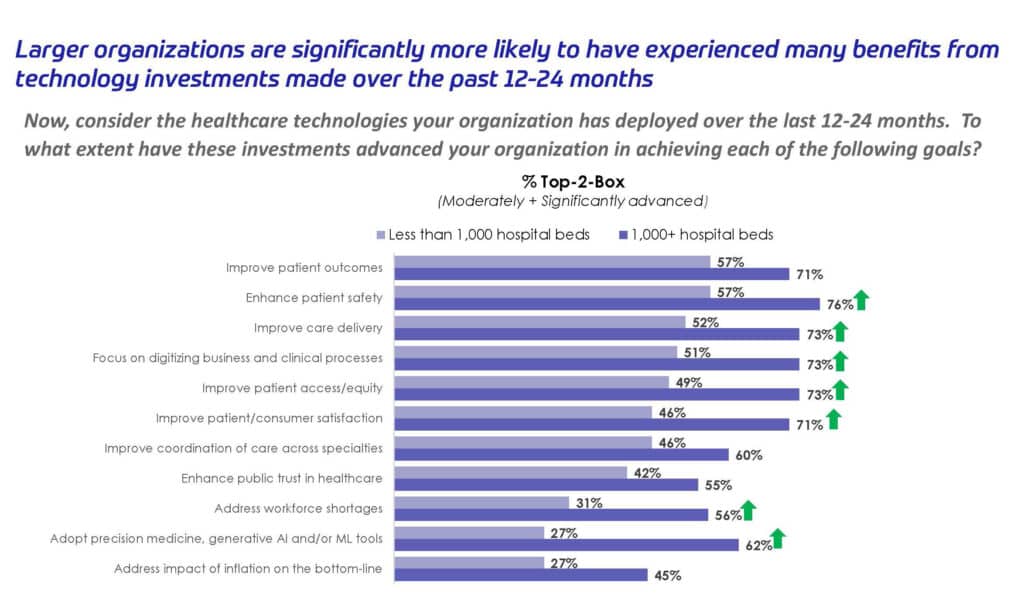
Because of these advantages, larger organizations are significantly more likely to experience more benefits from their tech investments.
Bridging financial barriers
Despite the advantages that larger health systems enjoy, smaller organizations can overcome financial barriers standing in the way of their digital transformation by:
- Prioritizing high-value initiatives. Approach every potential solution through the lens of ROI. Simply adopting new technologies is not enough; organizations need to track how their investments impact clinical, operational and financial outcomes.
- Taking a phased approach. Roll out digital transformation projects in stages, starting with smaller, more manageable investments that deliver quick wins. This helps build momentum and justify further investment, while giving organizations time to refine and improve as they evolve.
- Adopting cloud solutions. Cloud-based technologies often offer lower upfront costs and scalable pricing structures, making them more affordable for smaller organizations to deploy.
- Partnering to share the cost. Collaborate with vendors or other organizations to split the cost of technology investments. With a multi-tenant environment, for example, Consensus Cloud Solutions can easily provide digital cloud fax solutions to multiple entities who want to combine their buying power to share access to our technology.
While digital transformations can drain an organization’s resources—in terms of finances and labor—the benefits of change outweigh the struggle. At the risk of being left behind and pushed out of the market, even the smallest organizations will find a way to deploy the technologies they need to survive.
Maximizing the benefits of tech investments
Although they may not have access to the expansive budgets, sophisticated expertise or other deep resources that larger health systems enjoy, smaller healthcare organizations can maximize the benefits they reap from their tech investments by taking a strategic approach. This includes:
- Defining clear goals that are specific, measurable, achievable, relevant and time-bound (SMART)
- Focusing on user adoption by ensuring staff are properly trained and technologies are optimally integrated into user workflows
- Evaluating key metrics to assess how new technologies affect clinical outcomes, operational efficiency and financial performance
- Improving continuously by regularly reviewing metrics, identifying opportunities to optimize use and following through on feedback
- Embracing change by adopting a flexible mindset that allows evolution to happen and encourages people and processes to adapt
bviously, a smaller organization’s strategic priorities and path toward digital transformation will look much different than a larger health system’s journey. For example, the HIMSS survey showed that larger organizations are more likely to implement predictive analytics, big data and generative AI, while smaller organizations’ focus leans toward updating their legacy systems. What’s most important is that initiatives align with your strategic goals—showcasing the importance of cross-functional collaboration, as we discussed in the first blog of this series, Striking Alignment Around Health Tech Investments.
In the last installment of this series, we’ll analyze the results of the HIMSS survey to answer the ultimate question: Which tech investments deliver the biggest bang for the buck in healthcare?
Continue reading…
Part 1: Striking Alignment Around Health Tech Investments
Part 3: Prioritizing Health Tech Investments: Key Considerations for Leaders