As COVID-19 pushes our nation’s healthcare system to the brink, stories continue making headlines of how public health officials in many cities throughout the country are weeding through stacks of paper test results as they look to trace cases and quarantine patients. In other instances, people are waiting longer to find out if they have coronavirus because nasal swab test results are being paper faxed, which cause latency getting results into systems. To think we are relying on paper processes as the virus surges in many areas of our country is problematic. Add to the fact that 9 billion healthcare-related faxes were sent in 2018 (Nebergall, “Fax Technology is the Cornerstone of Interoperability. Here’s Why,” Open Health News, Feb. 6, 2019) and it is clear that now is the time for us to address healthcare’s Achilles’ heel – legacy paper communication systems.
Use of traditional paper fax, specifically the fax machine, is around because it is an established familiar technology that most people would agree works. After all, you can reliably send information from one person to another. However, when you are in the business of healthcare, your focus is on the quality and safety of patients and the thought of using new technologies can be a distraction which takes away from familiar workflows. Simply stated, the fax machine has proven itself year after year to be an easy way of sending and receiving information. But that doesn’t mean using paper fax the way many have been using it for decades is still the most efficient, convenient and secure way of sharing patient information between providers. If providers and public health officials are expected to stop using the fax machine as we know it, there needs to be an easy to use, reliable, affordable, secure technology that allows interoperability of all data for electronic health information to be shared.
An effective, secure and convenient alternative
The issue with paper faxes is the workflow and lack of system integration, which means added time for data to be actionable. Manual workflows needed to process paper documents are slow, laborious, error-prone and at times, incomplete. Paper faxing can be inexpensively replaced immediately with Digital Cloud Fax Technology (DCFT) which improves the digital transmission of information by eliminating paper, optimizing workflows and providing the ability for secure foundational interoperability.
For those unfamiliar with this technology, digital cloud fax is a secure, paperless, cost effective, and proven way for medical professionals to share documents and records. When professionally installed, it is HIPAA-compliant and falls into the Health Information Management Systems Society’s (HIMSS) category of “foundational interoperability.” Due to its simplicity and universal acceptance within healthcare, digital cloud fax technology is widely used in every setting with particular importance in communities that struggle to afford sophisticated electronic health-record systems, including public health, rural healthcare organizations and financially challenged urban clinics.
Compared to physical faxing, cloud faxing works like this: An employee creates an email, types in the recipient address, types a cover letter and hits “send.” The fax is sent securely into a determined workflow for an easy queue to manage documents, with a confirmation arriving a few minutes later. There is no printing, no scanning, no dialing, no waiting and no paper to file.
If a higher level of security is required, cloud faxing can transmit documents using TLS 1.2 and store them in a secure server with 256-bit encryption. Users log in to the server to view faxes.
Interoperability: the way forward
If interoperability of systems was easy and commonplace, faxing as we know it would be eliminated. Instead, data from disparate systems within a healthcare facility doesn’t always flow into the EHR, which means that same patient data stays behind as a patient move from provider to provider. Instead, connecting a provider’s EHR to its ambulatory physician EHRs, along with imaging, labs, pharmacy and more, requires specific connections between each system and the treating provider’s core EHR. Bringing data to a common platform multiplies the number of required connections exponentially.
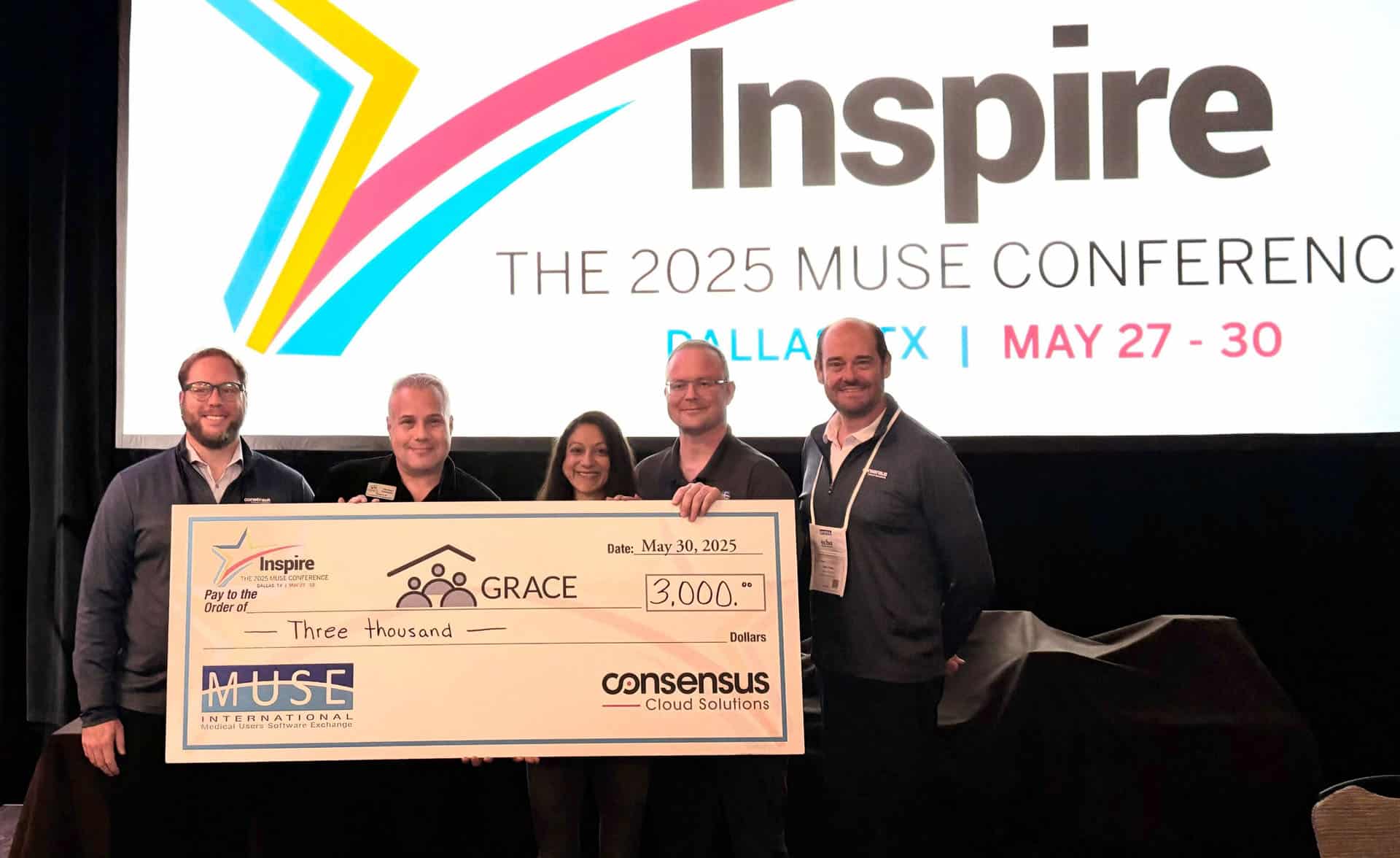
To help eliminate the continued burden paper holds on the healthcare industry, while at the same time helping make provider systems more interoperable, earlier this year, we introduced a platform that connects healthcare organizations through the continuum-of-care. Called Consensus, the platform offers one comprehensive connection with a simple, inbox-like dashboard to manage all incoming and outgoing patient documents including digital cloud faxes, Direct Secure Messaging, patient query and API integration into health exchange networks. With Consensus, providers can access leading EMR/EHR systems through CommonWell and Carequality, plus connections to ACOs and HIE data, allowing for the digital exchange of electronic health information between physicians, public health departments and labs.
Conclusion
Moving beyond paper eases operational and technological burdens that cause bottlenecks which impact patient care and threaten to cripple a public health system that has classically been underfunded by our nation’s healthcare system. What is happening with the lack of effective data sharing at several public health departments and what will undoubtedly happen elsewhere as the virus continues to surge in other areas of our county – including rural populations – can be avoided with a comprehensive interoperability system at our fingertips. One that integrates traditional faxing technology with efficient document management so that providers can exchange patient information electronically. And do so both safely and efficiently.